Female Urology
Urologic conditions affect both men and women, but women may experience disorders differently. Some urologic conditions, such as urinary incontinence (UI) and urinary tract infections (UTIs), are more common in women.
Urinary tract and kidney problems are common in women in part because the urinary tract is much closer to their genital area than in men. As such, pregnancy, childbirth and sexual intercourse can also play a part in urologic conditions affecting women.
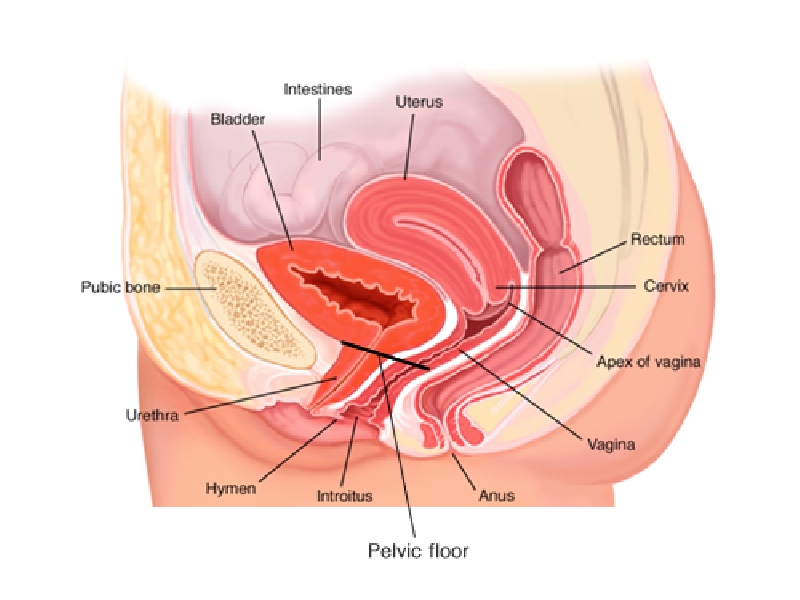
Female urological problems are due to diseases of the pelvic floor, bladder and urethra. The pelvic
floor includes the muscles, ligaments, connective tissue and nerves that support and help control the
bladder, vagina, uterus and rectum. Some common pelvic floor disorders are:
Leakage of urine (incontinence)
Overactive bladder (OAB), including frequent need to urinate, waking at night to urinate
(nocturia), strong urge to urinate (urgency)
Bulging, sagging or falling of pelvic organs (prolapse)
Painful urination (dysuria)
Painful intercourse (dyspareunia, vulvodynia)
Vaginal dryness
Painful bladder (interstitial cystitis, urethral syndrome)
Difficulty urinating or having bowel movements (emptying disorders)
These and other problems can result from childbirth, aging, illness, surgery, chronic constipation,
side effects of medications, repeated heavy lifting or other causes. A medical history, physical
examination and tests will help the urologist determine the cause of your problem and help you
decide on an appropriate treatment.
Listed below are common female urologic conditions:
- Urinary Incontinence – the accidental release of urine. There are three main types of chronic female urinary incontinence: stress incontinence, which occurs when you sneeze, cough, laugh, jog, or do other things that put pressure on your bladder; urge incontinence, which happens when you have a strong need to urinate but can’t reach the toilet in time; and overflow incontinence, which is an inability to completely empty your bladder.
- Overactive Bladder – the frequent and sudden urge to urinate.
- Voiding Dysfunction – the abnormality of the filling or emptying of the bladder. The three main types of chronic voiding dysfunction in women include: urinary frequency, urinary urgency, and painful urination.
- Urinary Tract Infection – an infection that usually occurs when bacteria enters the opening of the urethra and multiplies in the urinary tract.
- Bladder Infection – an infection that usually occurs when bacteria moves to the bladder and multiplies.
Interstitial Cystitis (IC) – a chronic inflammation of the bladder wall. - Pelvic Pain – pain, pressure, or tenderness around the pelvic region – below your bellybutton and between your hips.
- Bladder Cancer – any of several types of malignant growths of the urinary bladder.
- Bladder Pain – pain, pressure, or tenderness around the bladder, pelvis, and perineum – the area between the anus and vagina.
- Dropped Bladder (or prolapsed bladder) – the wall between a woman’s vagina and bladder weaken and the bladder drops into the vagina.
- Vaginal Prolapse – the organs inside the pelvis fall, bulge, or protrude into the vaginal wall.
- Urethral Syndrome – defined as symptoms suggestive of a lower tract urinary infection, without any evidence of bacterial or viral infection as a cause.
- Pelvic Organ Prolapse (cystocele, rectocele, enterocele, uterine prolapse)
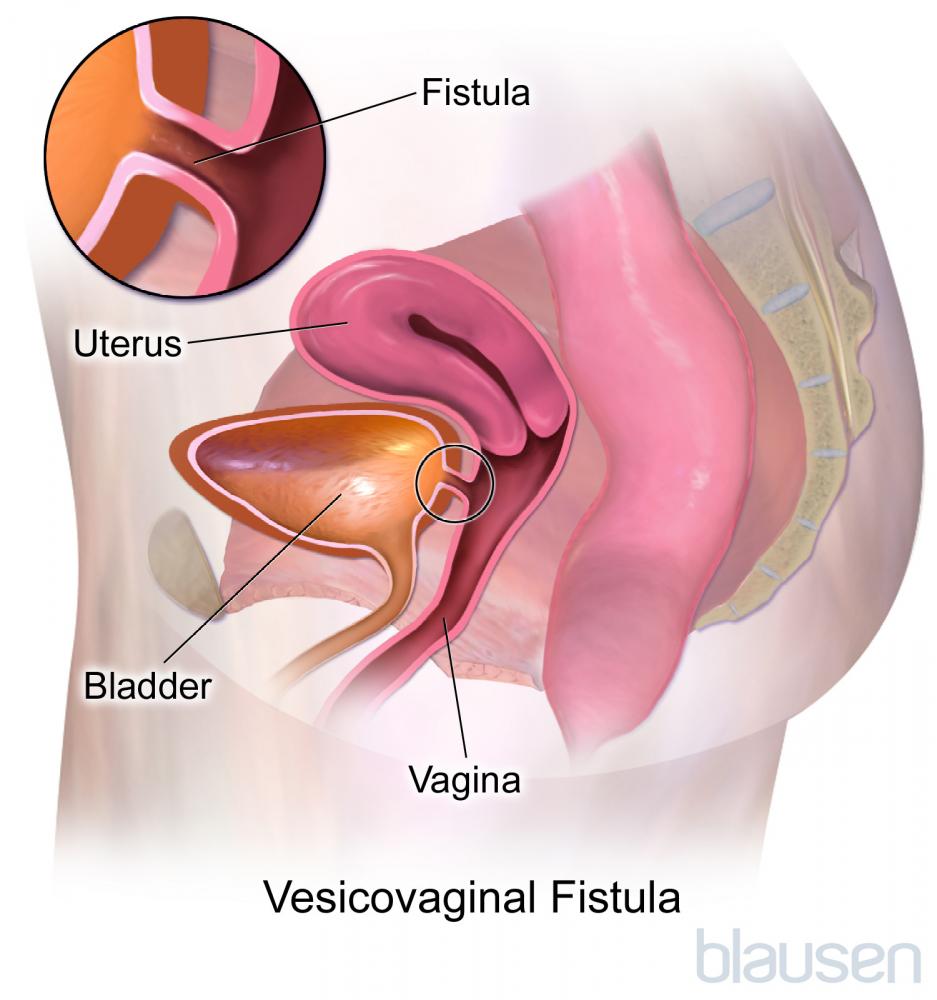
- Urinary Fistula (vesicovaginal fistula, urethral diverticula, urethral fistula)
- Nocturnal Enuresis
- Interstitial Cystitis
- Urethral Diverticula
Treatment Procedures
- Urinary Incontinence:
- Trans Obturator Tape (TOT):
- Vaginal sling surgery:
- Revision surgery for mesh complications:
- Sacral Neuromodulation:
- Botox® injections:
- Bladder enlargement (Augmentation cystoplasty):
- Pelvic Organ Prolapse:
- Vaginal repair (non mesh based) :
- Sacrocolpopexy (open or robotic assisted)
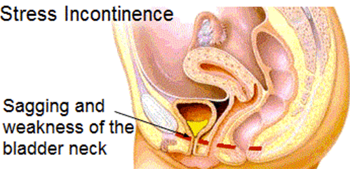
Stress Inconsistence
Urinary incontinence (UI) is defined by the International Continence Society as “the complaint of any involuntary loss of urine.” UI is a worldwide health problem that can significantly diminish an individual’s quality of life. Urinary incontinence (UI) is defined by the International Continence Society as “the complaint of any involuntary loss of urine.” UI is a worldwide health problem that can significantly diminish an individual’s quality of life.
UI is more common in women than in men. It has an increasing prevalence during young adult life, a broad peak around middle age, and then a steady increase in elderly women. Although variable, the prevalence of severe incontinence among most studies is estimated to be between 6% and 11%. The proportion of types of incontinence varies with age. In young and middle-aged women, stress incontinence predominates, and in older women mixed incontinence is most common. Over all age groups, stress incontinence is most common (49%) followed by mixed incontinence (29%) and pure urge incontinence (21%).
Signs and Symptoms
-
Stress urinary incontinence: is the complaint of involuntary leakage on exertion or with sneezing or coughing.
-
Urge urinary incontinence: is the complaint of involuntary leakage accompanied by or immediately preceded by a sudden compelling desire to urinate which is difficult to defer. Typically, this is described by patients as having a strong, sudden urge to urinate followed by running to get to the nearest bathroom, but often not making it in time, which may result in leakage of urine or complete bladder emptying.
-
Mixed urinary incontinence: is a combination of stress and urge incontinence.
Diagnosis
-
History: symptoms, duration, risk factors, impact on quality of life, medical history including previous surgeries, medications, allergies, and review of symptoms.
-
Physical exam: includes abdominal exam, pelvic examination paying special attention to vaginal support and urethral mobility, rectal exam, and limited neurologic examination.
-
Urinalysis/urine culture: analysis of urine to rule other causes of urinary symptoms such as a urinary tract infection.
-
Post void residual: a measurement of the volume retained in the bladder after a patient voids.
-
Intake/voiding/incontinence diary: a patient maintained diary measuring the amount of fluid consumed in a 24 hour period, the type of fluid, the number of voids, the volume of each void, the number of incontinence episodes, and related symptoms such as urinary urgency and pain.
-
Quality of life questionnaires: are validated assessments of the impact of urinary incontinence on a patient’s quality of life.
-
Pad testing: A pad is used to absorb lost urine during a predetermined length of time or after specific activities. The change in pad weight is an objective measurement of the severity of urinary incontinence and/or and may be used to assess the outcome of an intervention.
-
Urodynamics: is a test used to assess the storage and emptying ability of the bladder.
-
Cystourethroscopy: is an endoscopic evaluation of the urethra, bladder outlet, and bladder. This is used to rule out an anatomic or mucosal abnormality that may be contributing to urinary symptoms. This is most commonly done in the office.
Treatment – ACKU has been safely performing TOT- Tension Free Trans-obturator Tape operation with excellent outcome.
Vesicovaginal fistula
ACKU Treatment Options for VVF:
- Vaginal corrective repair:
- Abdominal corrective repair Laproscopically:
Quick Links
Contact Centre
- General enquiries
+88 02 9145809
+88 02 9145808
+88 01746 344179 - Request a call back
Can we call you back at a more convenient time - Email us
Send us an email enquiry and we will get back to you.